 Super bacteria, also referred to as superbugs, are bacteria that have grown resistant to most antibiotics. Overuse of antibiotics both in conventional livestock feed and in human medical applications has led to increasing bacterial resistance to antibiotic drugs. Microorganisms are weak creatures but they have their own way to protect their population and this is called mutation. A drug like penicillin targets an enzyme, and it’s easy for an organism to develop a single mutation to get past that. The development of new super bacteria types or mutation of the ones already known is of great unease to disease specialists. Concern exists that some strains could develop so much resistance to antibiotics that they would become virtually untreatable.
Super bacteria, also referred to as superbugs, are bacteria that have grown resistant to most antibiotics. Overuse of antibiotics both in conventional livestock feed and in human medical applications has led to increasing bacterial resistance to antibiotic drugs. Microorganisms are weak creatures but they have their own way to protect their population and this is called mutation. A drug like penicillin targets an enzyme, and it’s easy for an organism to develop a single mutation to get past that. The development of new super bacteria types or mutation of the ones already known is of great unease to disease specialists. Concern exists that some strains could develop so much resistance to antibiotics that they would become virtually untreatable.
When doctors prescribe the typical antibiotics for fighting an infection caused by super bacteria, the antibiotics usually fail to eradicate the bacteria. Instead, bacteria may actually thrive despite the medication, sometimes even killing the patient. To fight resistant bacteria, doctors often turn to even stronger antibiotics, but it seems that some super bacteria are developing the ability to thrive despite even the toughest antibiotic treatments. Bacteria that survive an antibiotic treatment produce new bacteria that may possess genetic structure to survive additional antibiotic treatments. Thus a new strain of the bacteria can be born and passed to other living organisms. Most of the super bacteria types are resistant to several antibiotics and could develop additional resistances in the future.
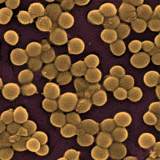
Unfortunately, much is still unknown about the exact mechanism involved, bacteria become resistant to antibiotics via chromosomal mutations and the incorporation of new genes, sometimes from other bacteria. There are already some super bacteria forms in existence that pose problems.  One of the best known of these is methicillin-resistant staphylococcus aureus (MRSA), which has until recently, been mostly noted in hospital and other medical settings.
One of the best known of these is methicillin-resistant staphylococcus aureus (MRSA), which has until recently, been mostly noted in hospital and other medical settings.  MRSA can cause serious external and internal infections that need specific antibiotic treatment. Generally start as small red bumps that resemble pimples, boils or spider bites. It can quickly turn into deep, painful abscesses that require surgical draining. Sometimes the bacteria remain confined to the skin. But bacteria can also penetrate into the body, potentially causing an infection that threatens the bones, joints, surgical wounds, bloodstream, heart valves and lungs, which in turn threatens a person’s soul. In the recent study, most cases of MRSA were treated with drugs that don’t work against the super bacteria.
MRSA can cause serious external and internal infections that need specific antibiotic treatment. Generally start as small red bumps that resemble pimples, boils or spider bites. It can quickly turn into deep, painful abscesses that require surgical draining. Sometimes the bacteria remain confined to the skin. But bacteria can also penetrate into the body, potentially causing an infection that threatens the bones, joints, surgical wounds, bloodstream, heart valves and lungs, which in turn threatens a person’s soul. In the recent study, most cases of MRSA were treated with drugs that don’t work against the super bacteria.
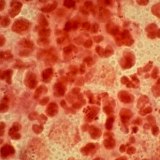
 Clostridium difficile (C. difficile) is a bacterium that causes mild to severe diarrhea and intestinal conditions like pseudomembranous colitis (or inflammation of the colon). When antibiotics destroy a person’s good bowel bacteria, C. difficile bacteria can grow. When this occurs, the C. difficile bacteria produce toxins, which can damage the bowel and cause diarrhea. However, some people can have C. difficile bacteria present in their bowel and not show symptoms. New data has revealed that infections from C. difficile are surpassing MRSA infections in community hospitals. C. difficile is spreading through hospitals and health care facilities, and it’s proving to be that C. difficile is more aggressive than the MRSA. C. difficile’s resistance to antibiotics allows it to spread easily through hospital. In fact, the drugs can actually increase the risk of getting the bacteria. Those antibiotics for their infection kill the bacteria that are normal in the bowel and C. difficile bacteria starts growing in the bowel.
Clostridium difficile (C. difficile) is a bacterium that causes mild to severe diarrhea and intestinal conditions like pseudomembranous colitis (or inflammation of the colon). When antibiotics destroy a person’s good bowel bacteria, C. difficile bacteria can grow. When this occurs, the C. difficile bacteria produce toxins, which can damage the bowel and cause diarrhea. However, some people can have C. difficile bacteria present in their bowel and not show symptoms. New data has revealed that infections from C. difficile are surpassing MRSA infections in community hospitals. C. difficile is spreading through hospitals and health care facilities, and it’s proving to be that C. difficile is more aggressive than the MRSA. C. difficile’s resistance to antibiotics allows it to spread easily through hospital. In fact, the drugs can actually increase the risk of getting the bacteria. Those antibiotics for their infection kill the bacteria that are normal in the bowel and C. difficile bacteria starts growing in the bowel.
Because MRSA is a Gram-positive, we don’t talk much here about the Gram-negatives — the two categories of bacteria have different cell-wall structures and thus are treated using different categories of drugs. (That structural difference causes them to react in different ways to a stain invented by a scientist named Gram in the 19th century.) But the resistance situation with Gram-negatives is at least as dire as with MRSA, possible more so, because there are fewer new drugs for Gram-negatives in the pharmacology pipeline.
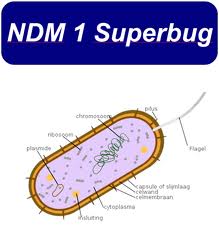 New Delhi metallo-beta-lactamase-1 (NDM-1) is an enzyme that makes bacteria resistant to a broad range of beta-lactam antibiotics. These include the antibiotics of the carbapenem family, which are a mainstay for the treatment of antibiotic-resistant bacterial infections. NDM-1 was first detected in a Klebsiella pneumoniae isolate from a Swedish patient of Indian origin in 2008. Klebsiella pneumoniae can cause different types of healthcare-associated infections, including pneumonia, bloodstream infections, wound or surgical site infections, and catheter-associated bladder infections.
New Delhi metallo-beta-lactamase-1 (NDM-1) is an enzyme that makes bacteria resistant to a broad range of beta-lactam antibiotics. These include the antibiotics of the carbapenem family, which are a mainstay for the treatment of antibiotic-resistant bacterial infections. NDM-1 was first detected in a Klebsiella pneumoniae isolate from a Swedish patient of Indian origin in 2008. Klebsiella pneumoniae can cause different types of healthcare-associated infections, including pneumonia, bloodstream infections, wound or surgical site infections, and catheter-associated bladder infections.
Klebsiella bacteria are normally found in the human intestines (where they do not cause disease) and in human stool (feces). In healthcare settings like hospitals and nursing homes, Klebsiella infections occur most commonly among very sick patients who are receiving treatment for serious conditions.  Klebsiella bacteria have developed resistance to antibiotics, most recently to the class of antibiotics known as carbapenems (carbapenem-resistant Klebsiella pneumoniae, or CRKP). CRKP is resistant to nearly all antibiotic options and has been associated with high mortality rates, long hospital stays, and high heathcare costs.
Klebsiella bacteria have developed resistance to antibiotics, most recently to the class of antibiotics known as carbapenems (carbapenem-resistant Klebsiella pneumoniae, or CRKP). CRKP is resistant to nearly all antibiotic options and has been associated with high mortality rates, long hospital stays, and high heathcare costs.
NDM-1 was later detected in bacteria in India, Pakistan, the United Kingdom, the United States, Canada, Japan and Brazil. The most common bacteria that make this enzyme are Gram-negative such as Escherichia coli and Klebsiella pneumoniae, but the gene for NDM-1 can spread from one strain of bacteria to another by horizontal gene transfer. The resistance factor has spread to 14 different species of bacteria, including pathogenic varieties responsible for dysentery and cholera. Most bacteria holding the NDM-1 plasmid are resistant to all but a couple of our most clumsy, brutal antibiotics. One strain is immune to all of them.
 Streptococcus pneumoniae is one of the world’s leading causes of death from infectious disease, particularly in children and the elderly. In the late 1970s, strains of pneumococci displaying resistance to penicillin were described in South Africa and Spain. By the early 1990s, penicillin-resistant clones of S. pneumoniae spread rapidly across Europe and globally. S. pneumoniae worldwide are multidrug-resistant (MDR) (i.e., resistant to ≥ 3 classes of antibiotics). The scariest sighting: Nine children in Rochester, N.Y., came down with a strain that shrugs off all 18 antibiotics approved for kids. The Rochester doctors who found the bug beat it into submission with Johnson & Johnson’s Levaquin, a drug for adults, but only after it left one child with permanent hearing loss.
Streptococcus pneumoniae is one of the world’s leading causes of death from infectious disease, particularly in children and the elderly. In the late 1970s, strains of pneumococci displaying resistance to penicillin were described in South Africa and Spain. By the early 1990s, penicillin-resistant clones of S. pneumoniae spread rapidly across Europe and globally. S. pneumoniae worldwide are multidrug-resistant (MDR) (i.e., resistant to ≥ 3 classes of antibiotics). The scariest sighting: Nine children in Rochester, N.Y., came down with a strain that shrugs off all 18 antibiotics approved for kids. The Rochester doctors who found the bug beat it into submission with Johnson & Johnson’s Levaquin, a drug for adults, but only after it left one child with permanent hearing loss.
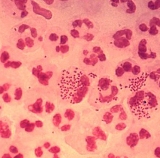 Gonorrhea is a very common infectious bacterium, a Gram negative, fastidious, diplococci, that can grow and rapidly multiply in the mucous membranes, especially the mouth, throat, and anus of males and females, and the cervix, fallopian tubes, and uterus of the female reproductive tract. Scientists have discovered a new form of gonorrhea in Japan that is resistant to all antibiotics that are used to treat the disease. Known as H041, the disease could become a worldwide epidemic if scientists are unable to find a way to eliminate its resistance to drugs. U.S. government health officials have warned that the sexually transmitted disease gonorrhea is becoming increasingly resistant to the last type of antibiotics left to treat it.
Gonorrhea is a very common infectious bacterium, a Gram negative, fastidious, diplococci, that can grow and rapidly multiply in the mucous membranes, especially the mouth, throat, and anus of males and females, and the cervix, fallopian tubes, and uterus of the female reproductive tract. Scientists have discovered a new form of gonorrhea in Japan that is resistant to all antibiotics that are used to treat the disease. Known as H041, the disease could become a worldwide epidemic if scientists are unable to find a way to eliminate its resistance to drugs. U.S. government health officials have warned that the sexually transmitted disease gonorrhea is becoming increasingly resistant to the last type of antibiotics left to treat it.
 Tuberculosis (TB) is an infectious disease caused by a germ called Mycobacterium tuberculosis. Tuberculosis is spread through the air when a person sneezes, coughs, or breathes. Both “multi-drug resistant (MDR)” and “extensively drug-resistant” forms of TB are now being seen. MDR Tuberculosis is resistant to at least two of the main drugs used to treat TB– isoniazid (INH), and rifampin.
Tuberculosis (TB) is an infectious disease caused by a germ called Mycobacterium tuberculosis. Tuberculosis is spread through the air when a person sneezes, coughs, or breathes. Both “multi-drug resistant (MDR)” and “extensively drug-resistant” forms of TB are now being seen. MDR Tuberculosis is resistant to at least two of the main drugs used to treat TB– isoniazid (INH), and rifampin.
 Neisseria meningitidis is a bacterium that can cause meningitis and other forms of meningococcal disease such as meningococcemia. N. meningitidis is a major cause of morbidity and mortality during childhood in industrialized countries and has been responsible for epidemics in Africa and in Asia. Meningitis is an inflammation of the membranes that cover the brain and spinal cord. People sometimes refer to it as spinal meningitis. Meningitis is usually caused by a viral or bacterial infection. Knowing whether meningitis is caused by a virus or bacterium is important because the severity of illness and the treatment differ depending on the cause. Viral meningitis is generally less severe and clears up without specific treatment. But bacterial meningitis can be quite severe and may result in brain damage, hearing loss, or learning disabilities. Although there have been reports of N. meningitidis with decreased susceptibility to penicillin.
Neisseria meningitidis is a bacterium that can cause meningitis and other forms of meningococcal disease such as meningococcemia. N. meningitidis is a major cause of morbidity and mortality during childhood in industrialized countries and has been responsible for epidemics in Africa and in Asia. Meningitis is an inflammation of the membranes that cover the brain and spinal cord. People sometimes refer to it as spinal meningitis. Meningitis is usually caused by a viral or bacterial infection. Knowing whether meningitis is caused by a virus or bacterium is important because the severity of illness and the treatment differ depending on the cause. Viral meningitis is generally less severe and clears up without specific treatment. But bacterial meningitis can be quite severe and may result in brain damage, hearing loss, or learning disabilities. Although there have been reports of N. meningitidis with decreased susceptibility to penicillin.
 Typhoid fever is a potentially fatal multisystemic illness caused primarily by Salmonella Typhi bacteria which is frequently multidrug resistant with reduced susceptibility to fluoroquinolone-based drugs, the first choice for the treatment of typhoid fever. S.Typhi has been a major human pathogen for thousands of years, thriving in conditions of poor sanitation, crowding, and social chaos. Untreated, typhoid fever is a grueling illness that may progress to delirium, obtundation, intestinal hemorrhage, bowel perforation, and death within one month of onset. Survivors may be left with long-term or permanent neuropsychiatric complications.
Typhoid fever is a potentially fatal multisystemic illness caused primarily by Salmonella Typhi bacteria which is frequently multidrug resistant with reduced susceptibility to fluoroquinolone-based drugs, the first choice for the treatment of typhoid fever. S.Typhi has been a major human pathogen for thousands of years, thriving in conditions of poor sanitation, crowding, and social chaos. Untreated, typhoid fever is a grueling illness that may progress to delirium, obtundation, intestinal hemorrhage, bowel perforation, and death within one month of onset. Survivors may be left with long-term or permanent neuropsychiatric complications.
 Enterococci are bacteria found in the stomach and bowels of about 19 out of every 20 healthy people. Enterococci can get into open wounds and skin ulcers, and cause infection. Less often, they can cause more serious infections of the blood or other body tissues. Vancomycin-Resistant Enterococci (VRE) are enterococci that have become resistant to vancomycin. Vancomycin is an antibiotic medication that is used to treat enterococcal infections. Some antibiotics do not work against some enterococci. Therefore, serious infections caused by VRE may be very hard to treat because they are resistant to vancomycin.
Enterococci are bacteria found in the stomach and bowels of about 19 out of every 20 healthy people. Enterococci can get into open wounds and skin ulcers, and cause infection. Less often, they can cause more serious infections of the blood or other body tissues. Vancomycin-Resistant Enterococci (VRE) are enterococci that have become resistant to vancomycin. Vancomycin is an antibiotic medication that is used to treat enterococcal infections. Some antibiotics do not work against some enterococci. Therefore, serious infections caused by VRE may be very hard to treat because they are resistant to vancomycin.
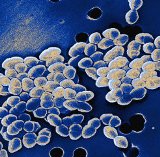
 Staphylococcus aureus is a bacterium commonly found on the skin and in the nose of about 30% of individuals. Most of the time, staph does not cause any harm. These infections can look like pimples, boils, or other skin conditions and most are able to be treated. Sometimes staph bacteria can get into the bloodstream and cause serious infections which can be fatal. Vancomycin-intermediate Staphylococcus aureus (VISA) and Vancomycin-resistant Staphylococcus aureus (VRSA) are specific types of antimicrobial-resistant bacteria.
Staphylococcus aureus is a bacterium commonly found on the skin and in the nose of about 30% of individuals. Most of the time, staph does not cause any harm. These infections can look like pimples, boils, or other skin conditions and most are able to be treated. Sometimes staph bacteria can get into the bloodstream and cause serious infections which can be fatal. Vancomycin-intermediate Staphylococcus aureus (VISA) and Vancomycin-resistant Staphylococcus aureus (VRSA) are specific types of antimicrobial-resistant bacteria.
 Shigella is the bacterium that causes shigellosis, a diahrreal disease, also known as bacillary dysentery. Shigella is one of the most easily transmitted bacterial diarrheas, since it can occur after fewer than 100 bacteria are ingested. Shigella bacteria are generally transmitted through a fecal-oral route. Foods that come into contact with human or animal waste can transmit Shigella. Thus, handling toddlers’ diapers, eating vegetables from a field contaminated with sewage, or drinking pool water are all activities that can lead to shigellosis. In the developed world, shigellosis typically isn’t considered dangerous. To shorten the length of illness and to reduce potential infection of other people, antibiotics are typically prescribed, usually cotrmoxazole or ampicillin. Over the decades, Shigella isolates resistant to multiple agents, resulting in difficulties in the selection of empirical therapy.
Shigella is the bacterium that causes shigellosis, a diahrreal disease, also known as bacillary dysentery. Shigella is one of the most easily transmitted bacterial diarrheas, since it can occur after fewer than 100 bacteria are ingested. Shigella bacteria are generally transmitted through a fecal-oral route. Foods that come into contact with human or animal waste can transmit Shigella. Thus, handling toddlers’ diapers, eating vegetables from a field contaminated with sewage, or drinking pool water are all activities that can lead to shigellosis. In the developed world, shigellosis typically isn’t considered dangerous. To shorten the length of illness and to reduce potential infection of other people, antibiotics are typically prescribed, usually cotrmoxazole or ampicillin. Over the decades, Shigella isolates resistant to multiple agents, resulting in difficulties in the selection of empirical therapy.
 Acinetobacter bacteria are present in water, soil and sewage. Acinetobacter is causing severe bloodstream infection and pneumonia in many hospital patients. Acinetobacter infections are uncommon but, when they occur, usually involve organ systems that have a high fluid content (eg, respiratory tract, CSF, peritoneal fluid, urinary tract), manifesting as nosocomial pneumonia, infections associated with continuous ambulatory peritoneal dialysis (CAPD), or catheter-associated bacteruria. Multi-drug resistant (MDR) Acinetobacter is not a new or emerging phenomenon. Since the 1970s, the spread of MDR Acinetobacter strains among critically ill, hospitalized patients, and subsequent epidemics, have become an increasing cause of concern.
Acinetobacter bacteria are present in water, soil and sewage. Acinetobacter is causing severe bloodstream infection and pneumonia in many hospital patients. Acinetobacter infections are uncommon but, when they occur, usually involve organ systems that have a high fluid content (eg, respiratory tract, CSF, peritoneal fluid, urinary tract), manifesting as nosocomial pneumonia, infections associated with continuous ambulatory peritoneal dialysis (CAPD), or catheter-associated bacteruria. Multi-drug resistant (MDR) Acinetobacter is not a new or emerging phenomenon. Since the 1970s, the spread of MDR Acinetobacter strains among critically ill, hospitalized patients, and subsequent epidemics, have become an increasing cause of concern.
 Group B streptococci (GBS) are found commonly in the gastrointestinal tract and have been found to colonize the urethra in both men and women without causing infection. GBS can also colonize the upper respiratory tract. GBS are the leading cause of serious, life-threatening infections (pneumonia, septicemia, and meningitis) in the newborn. Mortality of GBS sepsis in neonates is over 50% and is particularly high in preterm infants. GBS colonize the vaginal and gastrointestinal tracts in healthy women, with carriage rates ranging from 15%-45%. The absence of antibody to GBS in infants is a risk factor for infection. GBS infection in elderly people (≥70 y) is strongly linked to congestive heart failure and being bedridden, with urinary tract infection, pneumonia, and soft-tissue infection as the most common manifestations of infection. Erythromycin and clindamycin are the drugs of choice for women with serious penicillin allergy who are colonized with GBS. But the prevalence of resistance to clindamycin and erythromycin is high.
Group B streptococci (GBS) are found commonly in the gastrointestinal tract and have been found to colonize the urethra in both men and women without causing infection. GBS can also colonize the upper respiratory tract. GBS are the leading cause of serious, life-threatening infections (pneumonia, septicemia, and meningitis) in the newborn. Mortality of GBS sepsis in neonates is over 50% and is particularly high in preterm infants. GBS colonize the vaginal and gastrointestinal tracts in healthy women, with carriage rates ranging from 15%-45%. The absence of antibody to GBS in infants is a risk factor for infection. GBS infection in elderly people (≥70 y) is strongly linked to congestive heart failure and being bedridden, with urinary tract infection, pneumonia, and soft-tissue infection as the most common manifestations of infection. Erythromycin and clindamycin are the drugs of choice for women with serious penicillin allergy who are colonized with GBS. But the prevalence of resistance to clindamycin and erythromycin is high.
When we read or hear the word “bacteria” we often think of getting sick. However, not all bacteria are harmful. Some bacteria are very helpful to humans. Bacteria are involved in the production of fuel, food, and medications. Bacteria are also used in environmental recycling and clean-up. In fact, without certain bacteria, human life would be a lot more difficult. The human body is full of helpful bacteria. The human digestive tract is full of these helpful bacteria. Essentially, these bacteria serve two purposes – they help prevent other harmful bacteria from growing and they help humans digest their food. These bacteria work with the body’s own chemicals in breaking down food, converting it to useful vitamins and minerals, and making sure the intestinal walls can absorb the nutrients for the bloodstream to circulate. Human skin contains many species of harmless bacteria. Their presence prevents harmful bacteria from gaining a foothold on your skin. In fact, if it wasn’t for certain bacteria in your body, you would become ill. Unfortunately most of the people are at war with all bacteria. Keep this in mind. Avoid using any unnecessary antibiotics.
Modern medicine certainly have an important place in treatment. Most Doctors of Medicine, are dedicated, clever people doing wonderful work, but sometimes the treatment is hopeless, or, even worse than the problem. When you get a multi-drug resistant (MDR) strain of super bacteria, what can you do about it? First, stop worrying about it. Our bodies do a great job at fighting the germ war for us! We need some alternate ways to treat these infections. We need to pay attention to our biological design not disease. Drugs override normal immune system cell processes and the problem is not resolved. It is possible to prevent the spread of the MDR super bacteria in the body without the use of typical antibiotics. It is possible to strengthen, balance and boost your immune system with natural non toxic agents and build it up into your body’s best defense mechanism your immune system.
 The immune system is an intricate complex of interrelated cellular, molecular, and genetic components that is responsible for protecting us against infections and foreign substances. A healthy immune system can defeat invading super bacteria. Specific nutrients, immune molecules and bio-factors support immune system cell processes and address’s the immune system dysfunctions. Key immune system health supports a cascade of immune responses that begin in the mouth and proceed throughout the body and it optimizes response of natural killer cells, B-cells and T-cells, which seek out and destroy foreign substances. So your body can maximize its immune system functions and eradicate super bacteria. Hepazym may be our best weapon in the fight against MDR super-bacterial infection. It could save your life. Hepazym is much more specific than more antibiotics, so it can be chosen to be harmless not only to the humans, but also to other beneficial bacteria, such as gut flora, reducing the chances of opportunistic infections. It would have a high therapeutic index, that is, Hepazym-therapy would not be expected to give rise to unwanted side effects, as opposed to drugs, and would not stress the liver. It will only kill a harmful bacterium. Hepazym is currently being used therapeutically to treat super-bacterial infections that do not respond to conventional antibiotics. It tend to be more successful than any antibiotics.
The immune system is an intricate complex of interrelated cellular, molecular, and genetic components that is responsible for protecting us against infections and foreign substances. A healthy immune system can defeat invading super bacteria. Specific nutrients, immune molecules and bio-factors support immune system cell processes and address’s the immune system dysfunctions. Key immune system health supports a cascade of immune responses that begin in the mouth and proceed throughout the body and it optimizes response of natural killer cells, B-cells and T-cells, which seek out and destroy foreign substances. So your body can maximize its immune system functions and eradicate super bacteria. Hepazym may be our best weapon in the fight against MDR super-bacterial infection. It could save your life. Hepazym is much more specific than more antibiotics, so it can be chosen to be harmless not only to the humans, but also to other beneficial bacteria, such as gut flora, reducing the chances of opportunistic infections. It would have a high therapeutic index, that is, Hepazym-therapy would not be expected to give rise to unwanted side effects, as opposed to drugs, and would not stress the liver. It will only kill a harmful bacterium. Hepazym is currently being used therapeutically to treat super-bacterial infections that do not respond to conventional antibiotics. It tend to be more successful than any antibiotics.